Vaccines are essential defences against the various pathogens that swarm this planet and target our health. Early attempts to prevent diseases like smallpox were practiced in China, India and the Middle East and involved inoculation (or variolation), which meant causing a mild infection (with smallpox) in order to create immunity. In the 1720s, this was introduced to the US and England.
Inoculation involved serious risks of infection in the patient, as well as of infecting others. In 1798, Edward Jenner created the first ever vaccine and used it successfully. He had observed that milkmaids were generally immune to smallpox and realised that this was because they had been infected with the much less virulent cowpox. He then used this to develop the vaccine for smallpox. This meant that the dangers of inoculations – actually infecting the patient with smallpox – were curtailed significantly.
Moving on to the 20th century and a host of vaccinations were developed based on their life saving properties, including the polio vaccine created by Jonas Edward Salk in 1955. (Side note: the world’s first polio vaccine was successfully demonstrated by Hilary Koprowsky in 1950 but it did not take off because it used a live polio virus. Salk used inactive or killed viruses). Smallpox was eventually completely eradicated and polio is almost gone too. Other diseases like measles and whooping cough have been successfully contained. Diseases caused by Haemophilus influenza have decreased by 99% in the USA, since the introduction of the vaccine in 1988. A vaccine for the Ebola virus shows promise.
(Read What are Zoonotic Diseases and A Brief History of Pandemics)
What are vaccines?
Vaccines are the best means for a population to acquire herd immunity without causing untold fatalities that might result from natural herd immunity. A vaccine typically contains a biological prepration made from the inactivated infectious agent (antigen), or a synthetic one that mimics the infection. When delivered into the human body, this prepration causes cells to produce the relevant pathogen protein (without actually causing the disease) and thus trains the body to ramp up its immune responses quickly.
What are mRNA vaccines?
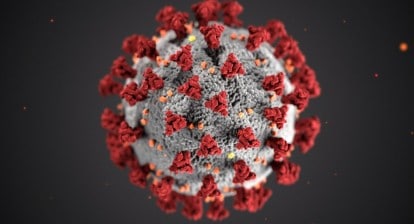
Scientists have been working to bring out vaccines to shore-up our defences against Sars-Cov-2 – the virus that has spread across the planet, mutating at break-neck speed. The success of this global effort has resulted in many contenders, two of which are known as mRNA vaccines. This is a novel type of vaccine, composed of the nucleic acid RNA, packaged inside tiny fat droplets, known as lipid nanoparticles (LNPs). These vaccines also mimic the infection but in a completely different, more robust and effecient way, making them more versatile than the traditional methods. RNA are messenger molecules (they are NOT the genetic code or DNA of the virus!), that carry genetic information to the cell, enabling it to synthesise proteins (such as the spike protein of Sars-Cov-2). An analogy by Harvard University’s Science in the News magazine explains it thus: “one can see the DNA as a cook book in a library: the recipe is stored here but cannot be used. The commis, or chef’s assistant, first makes a copy (the RNA) of a specific recipe and brings it to the kitchen. The information is now ready-to-use by the chef, who can add the ingredients in the order specified by the recipe and create a cake (the protein).”

mRNA Vaccine Technology. Source: SITNBoston, Harvard University CC.BY
(Read Are Antivaxxers Right?)
How does the mRNA vaccine work?
In this type of vaccination, instead of the antigent (infection agent), RNA carrying the antigen is introduced into the body. This messenger RNA (mRNA) has the genetic code and instructions for the cell to produce the antigen itself. Once the antigen has been produced, the body reacts in the same way it would with traditional vaccines. Cells remember the foreign protein (infection agent or antigen) and if the actual infection enters the body, its immune response acts quickly to kill it via antibodies and T-Cells. The injection of RNA presents no danger of damaging or disrupting the cell’s natural DNA sequence. Continuing with the Harvard analogy “it is like temporarily adding a new recipe in the cook book while keeping old ones untouched, and therefore will not result in surprising changes to existing recipes”.
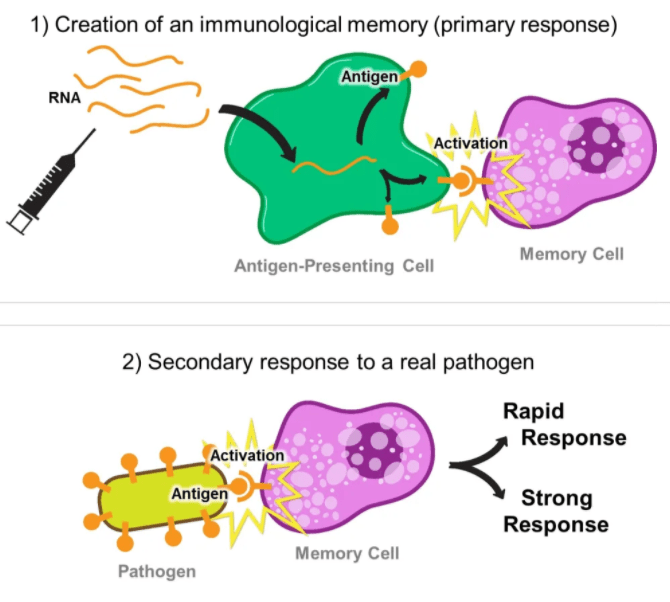
mRNA Vaccine Disease Prevention. Source: SITNBoston, Harvard University CC.BY
How are mRNA vaccines produced?
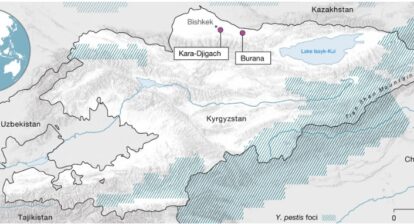
Over the past few decades significant advances have been made in decoding the genetic sequences of organisms, including of pathogens like coronavirus. Its genetic sequence was shared by Chinese scientists in January 2020, soon after infection rates started rising. Scientists use the relevant antigen coding segment of the DNA from pathogens (including from coronavirus), and together with some engineering to produce the relevant mRNA, insert this into a LNP template. The whole package is then introduced into the human body. This method is quick and its verstatility means any vaccine can be created in this way, such as a universal flu shot and an HIV vaccine. More importantly RNA vaccines can contain information for more than one antigen in one dose; for example a number of flu mutations can be included, precluding the necessity of annual shots.
What are the shortcomings of RNA vaccines?
The most important one has already been made clear: that of cold storage. Companies are now looking at developing vaccines that would not need such cold temperatures as those by Pfizer-BioNtech and Moderna.
They also require a double dose; another potentially problematic issue, since people may neglect taking the second dose. The Covid19 pandemic has given impetus to RNA vaccine research and scientists/ companies are looking at ways to come up with smaller or single dosage options. An example is that of a self-replicating RNA strand that would make more copies of the antigen, promoting a stronger immune response with just one dose.
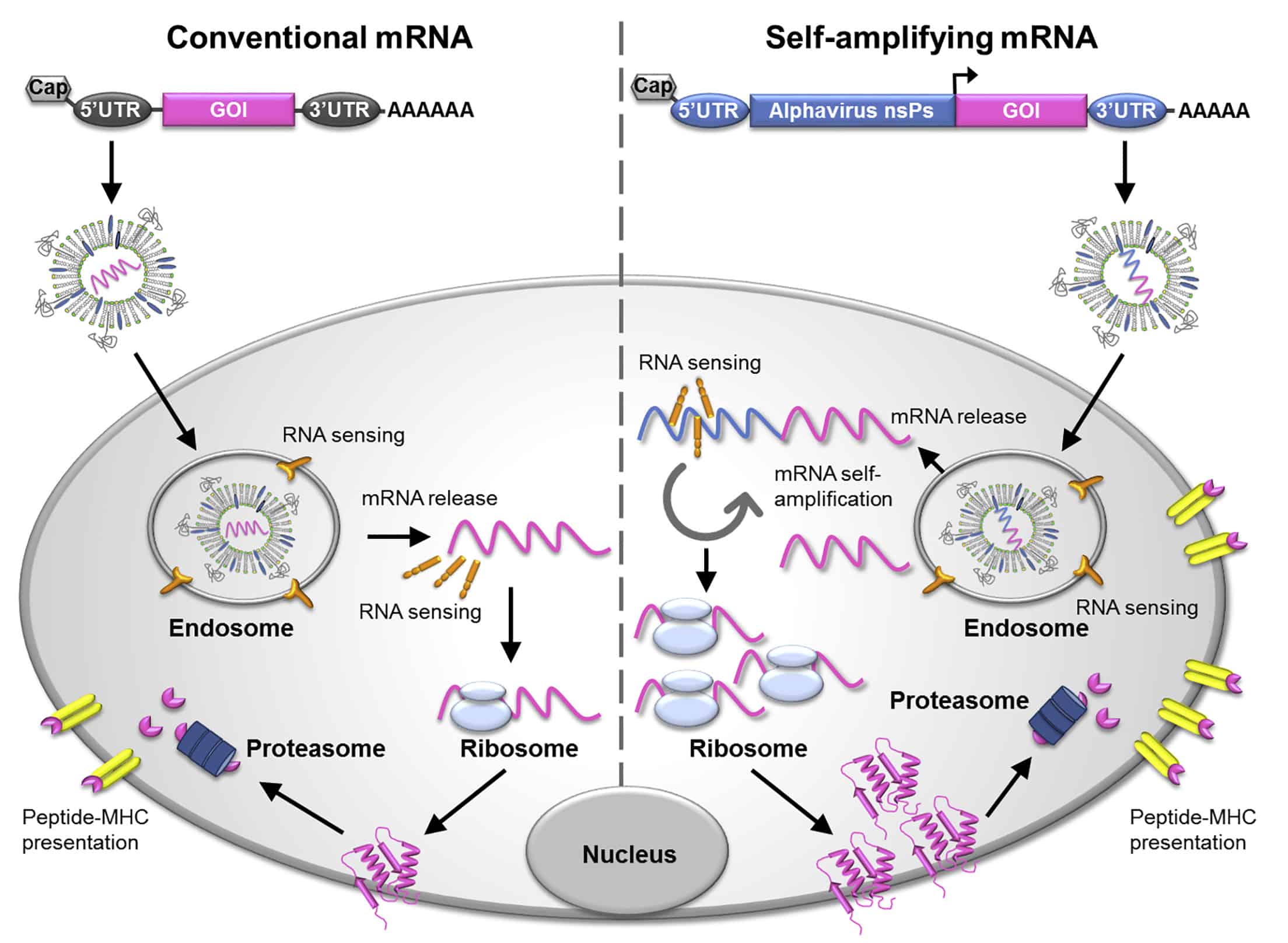
Conventional and Self-replicating mRNA. © 2019 The American Society of Gene and Cell Therapy.
Analogy and image 1 and 2 source: SITNBoston, Harvard University